Research progress on biological targets of traditional Chinese medicine in the treatment of diarrhea predominant irritable bowel syndrome
Diarrhea predominant irritable bowel syndrome (IBS-D) is the most common subtype of irritable bowel syndrome (IBS), characterized by diarrhea, abdominal pain, and discomfort. IBS-D belongs to the category of “diarrhea” in traditional Chinese medicine research, and its location is in the gastrointestinal tract. Today, the global incidence rate of IBS is 11%, and the incidence rate of IBS-D accounts for 23.4% of IBS. The pathogenesis of IBS-D is relatively complex. According to modern medical research, it is now known that the formation of IBS-D is related to factors such as gastrointestinal inflammation, increased visceral sensitivity, abnormal brain gut axis, disrupted intestinal microbiota, and damaged intestinal barrier. These pathological mechanisms will have an impact on the occurrence and development of IBS-D. There are many key signaling factors and signaling pathways in the pathological process of IBS-D, which can be used as key biological targets for the treatment of IBS-D (see Figure 1). By inhibiting, activating or regulating these biological targets, it is beneficial to reduce the incidence rate of IBS-D and improve the therapeutic effect of drugs.
The occurrence and development of IBS-D involve multiple pathogenic factors, which can stimulate the gastrointestinal tract and cause intestinal damage. Moreover, the course of IBS-D is relatively long, which has adverse effects on the physical and mental health of patients. Western medicine usually uses drugs such as povidonium bromide, allosetron, iludoxine, and rifampicin to treat IBS-D, but there are disadvantages such as large side effects and easy recurrence of the disease after discontinuation. Moreover, the treatment effect of Western medicine alone is not satisfactory. The selection of traditional Chinese medicine intervention for the treatment of IBS-D is considered a safe and effective method in clinical practice. Traditional Chinese medicine and its compound have shown significant therapeutic effects on IBS-D, and the use of traditional Chinese medicine in the treatment of IBS-D is superior to Western medicine in improving patients’ clinical symptoms. In addition, through the formulation of traditional Chinese medicine formulas, treatment can be carried out according to the differences in patients’ symptoms, achieving the therapeutic effect of syndrome differentiation and treatment. This article reviews the latest research progress on the biological targets of traditional Chinese medicine in the treatment of IBS-D related gastrointestinal inflammation, increased visceral sensitivity, brain gut axis abnormalities, intestinal microbiota disorders, and intestinal barrier damage.
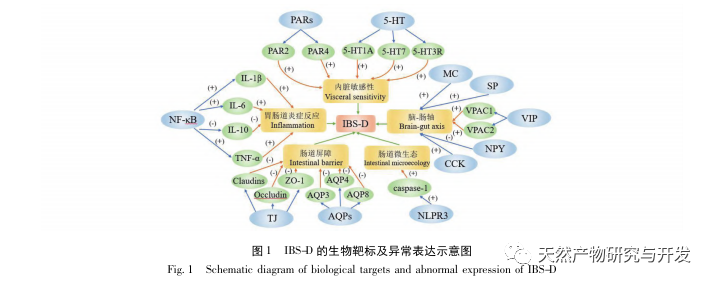
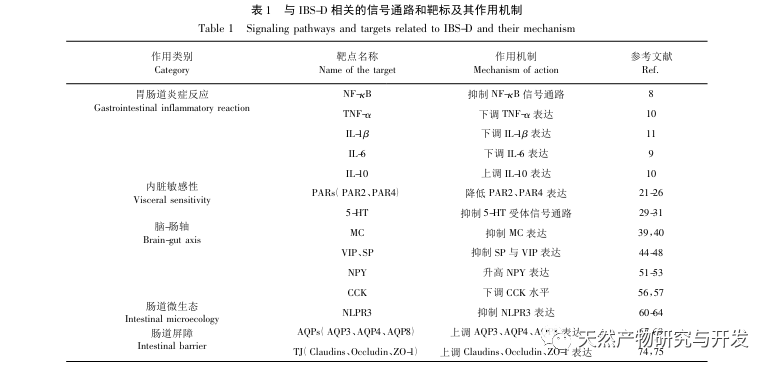
 IBS-D is a common gastrointestinal disease in the population. The pathogenesis of IBS-D is complex, and according to current research trends, factors such as gastrointestinal inflammation, increased visceral sensitivity, abnormal brain gut axis, disruption of intestinal microbiota, and damage to intestinal barrier are considered the main causes of IBS-D. There are multiple key pathways and signaling factors involved in the pathogenesis of IBS-D, which serve as objective indicators for detecting IBS-D and important biological targets for treating IBS-D. By studying the key targets in the pathological mechanism of IBS-D regulated by traditional Chinese medicine and its formulas, it is suggested that traditional Chinese medicine has a significant therapeutic effect on gastrointestinal inflammation by inhibiting the NF – κ B signaling pathway and inflammatory factors such as TNF – α, IL-1 β, IL-6, and upregulating the expression of anti-inflammatory factor IL-10; Reducing the expression of PAR2 and PAR4 and inhibiting the 5-HT receptor signaling pathway can alleviate visceral hypersensitivity; By inhibiting MC and regulating the expression levels of brain gut peptide hormones VIP, SP, NPY, and CCK in the brain gut axis, the brain gut axis can be regulated; Inhibiting NLPR3 expression can improve gut microbiota disorder and regulate gut microbiota; In addition, the expression of AQPs in the intestine can be upregulated to regulate water metabolism, and the expression of Claudins, Occludin, and ZO-1 can be upregulated to restore intestinal mucosal TJ and achieve the goal of restoring intestinal barrier (see Table 1). Traditional Chinese medicine and its compound formulas have shown significant therapeutic effects on IBS-D, which can significantly improve clinical symptoms such as diarrhea, abdominal pain, and discomfort, alleviate patients’ physical and mental pain, and Chinese medicine is significantly superior to Western medicine in both efficacy and side effects in the treatment of IBS-D.
IBS-D is a common gastrointestinal disease in the population. The pathogenesis of IBS-D is complex, and according to current research trends, factors such as gastrointestinal inflammation, increased visceral sensitivity, abnormal brain gut axis, disruption of intestinal microbiota, and damage to intestinal barrier are considered the main causes of IBS-D. There are multiple key pathways and signaling factors involved in the pathogenesis of IBS-D, which serve as objective indicators for detecting IBS-D and important biological targets for treating IBS-D. By studying the key targets in the pathological mechanism of IBS-D regulated by traditional Chinese medicine and its formulas, it is suggested that traditional Chinese medicine has a significant therapeutic effect on gastrointestinal inflammation by inhibiting the NF – κ B signaling pathway and inflammatory factors such as TNF – α, IL-1 β, IL-6, and upregulating the expression of anti-inflammatory factor IL-10; Reducing the expression of PAR2 and PAR4 and inhibiting the 5-HT receptor signaling pathway can alleviate visceral hypersensitivity; By inhibiting MC and regulating the expression levels of brain gut peptide hormones VIP, SP, NPY, and CCK in the brain gut axis, the brain gut axis can be regulated; Inhibiting NLPR3 expression can improve gut microbiota disorder and regulate gut microbiota; In addition, the expression of AQPs in the intestine can be upregulated to regulate water metabolism, and the expression of Claudins, Occludin, and ZO-1 can be upregulated to restore intestinal mucosal TJ and achieve the goal of restoring intestinal barrier (see Table 1). Traditional Chinese medicine and its compound formulas have shown significant therapeutic effects on IBS-D, which can significantly improve clinical symptoms such as diarrhea, abdominal pain, and discomfort, alleviate patients’ physical and mental pain, and Chinese medicine is significantly superior to Western medicine in both efficacy and side effects in the treatment of IBS-D.
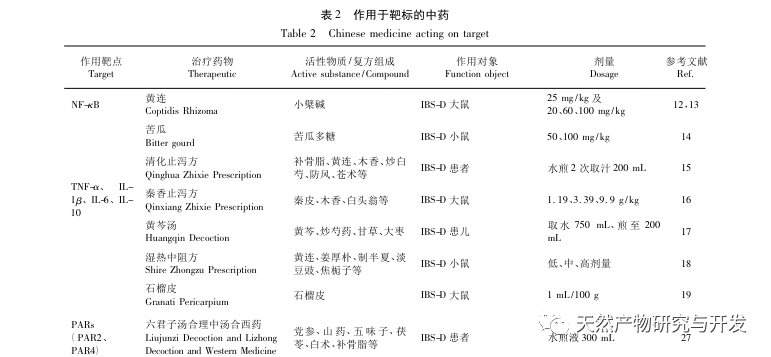
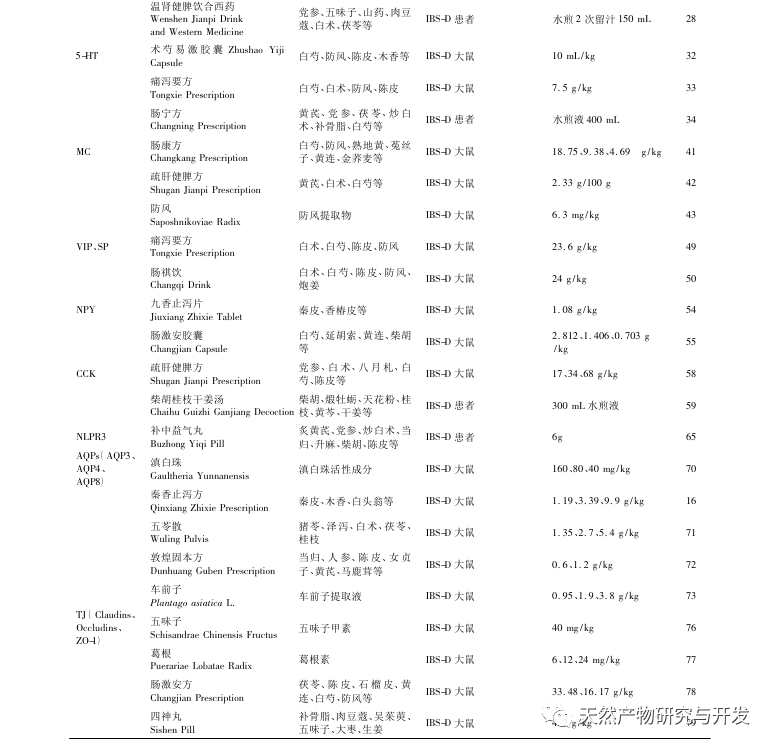
Traditional Chinese medicine research divides IBS-D into multiple syndrome types based on the method of syndrome differentiation and treatment, mainly including liver depression and spleen deficiency syndrome, spleen stomach damp heat syndrome, spleen deficiency and dampness obstruction syndrome, spleen kidney yang deficiency syndrome, etc. For various types of syndromes, different traditional Chinese medicines and formulas have regulatory effects on their related biological targets. Through studying the traditional Chinese medicines that act on various targets (see Table 2), it was found that the Chinese medicines with high frequency of occurrence in the treatment of IBS-D include Huanglian and Huangqin, which mainly have the function of clearing heat and dampness; Astragalus membranaceus and Atractylodes macrocephala, which have the main function of tonifying qi and spleen; Paeonia lactiflora, which has the main function of softening the liver and relieving pain, belongs to the liver and spleen meridians; Chenpi, which has the main function of regulating qi and strengthening spleen; Yam with the main function of tonifying the spleen and kidneys; The main function is to warm the kidneys and promote yang, and it enters the spleen and kidney meridians through the use of psoralen. The formation of IBS-D is mainly related to spleen and stomach disorders, with spleen and stomach damp heat and liver depression and spleen deficiency being the main causes of IBS-D. Traditional Chinese medicine therapies such as soothing the liver and strengthening the spleen, drying dampness and strengthening the spleen, warming the kidneys and tonifying the spleen are of great significance for the treatment of IBS-D. Therefore, further research on the regulation of IBS-D related biological targets by traditional Chinese medicine and its compound formulas can also be conducted from the perspective of TCM syndrome differentiation and treatment.
Despite the complex pathogenesis of IBS-D and the urgent need for improvement in related research, multiple omics analyses have been conducted on IBS-D patients, revealing for the first time that the microbial purine metabolism pathway plays an important role in the pathogenesis of IBS-D, providing multiple new potential targets for the treatment of IBS-D. Therefore, from a long-term research perspective, as the understanding of the pathogenesis of IBS-D deepens, its pathological process is influenced by multiple key signaling pathways and the expression of biomarkers. The future development direction of research and treatment for IBS-D may be closely related to its key biological targets. Traditional Chinese medicine has a significant regulatory effect on the key biological targets of IBS-D. By classifying and summarizing the key biological targets involved in the treatment of IBS-D with traditional Chinese medicine, and based on the regulatory, activating, or inhibitory effects of traditional Chinese medicine and its formulas on different biological targets, these key targets can serve as a theoretical basis for studying the treatment of IBS-D. Therefore, research on the treatment of IBS-D can provide traditional Chinese medicine solutions for the prevention and treatment of IBS-D by strengthening the connection with traditional Chinese medicine diagnosis and treatment plans, based on regulating its key biological targets.
