The Mechanism of Artesunate Alleviating Spleen Fibrosis in Type 2 diabetes Rats Based on TGF – β/Smad Pathway
Type 2 diabetes (T2DM) is a chronic metabolic disease. As the incidence rate of T2DM continues to rise, it has become the third chronic disease threatening human health in the world. In addition, the incidence rate and prevalence of young people are on the rise worldwide. If not treated in time, a series of serious diseases and target organ damage will occur, which will shorten the life of diabetes patients. When high blood sugar levels in T2DM patients cause oxidative stress and elevated levels of inflammatory factors, it can lead to splenic cell apoptosis and immune dysfunction, ultimately resulting in splenic damage. At the same time, excessive inflammatory response can cause splenic fibrosis, and the proliferation of collagen fibers can further restrict splenic blood supply, causing irreversible damage to patients. However, there is currently no effective method for preventing and treating splenic damage and fibrosis in T2DM patients. However, transforming growth factor beta (TGF – β) and its main pathway TGF – β/Smad are closely related to fibrosis progression. Studies have shown that TGF – β/Smad plays an important regulatory role in fibrosis processes in various organs such as pulmonary fibrosis, renal fibrosis, liver fibrosis, and pancreatic fibrosis. However, there are few reports at home and abroad on whether it is related to splenic fibrosis.
Artesunate (ART), a natural sesquiterpene lactone compound extracted from artemisinin, a Chinese herbal medicine, is a first-line treatment drug for antimalarial agents. In recent years, research has also found that ART has anti-tumor, immune regulation, anti-virus, anti fibrosis and other effects. In the early research of the research group, it was found that ART can not only reduce the blood sugar of diabetes rats, but also have a preventive effect on kidney, lung fibrosis and oxidative stress. However, whether ART has an impact on the spleen tissue of T2DM and its fibrosis has not been studied, and its related mechanism has not been revealed. Therefore, this experiment is to observe the effect of ART on the spleen structure and fibrosis of T2DM rats by establishing a T2DM rat model. And explore whether it may be related to TGF – β/Smad pathway.
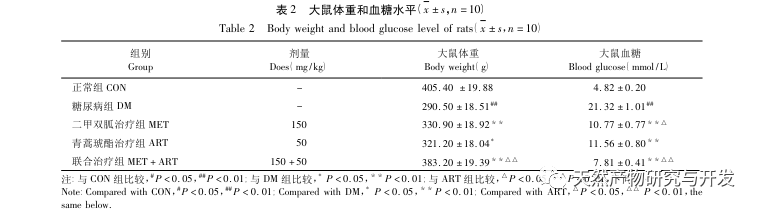
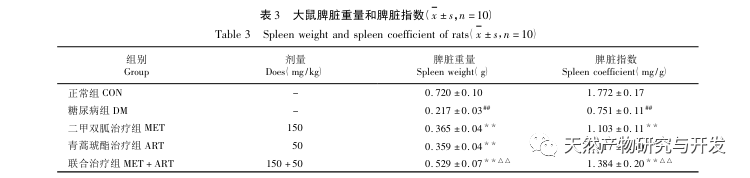
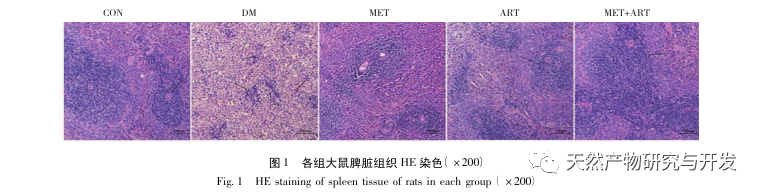
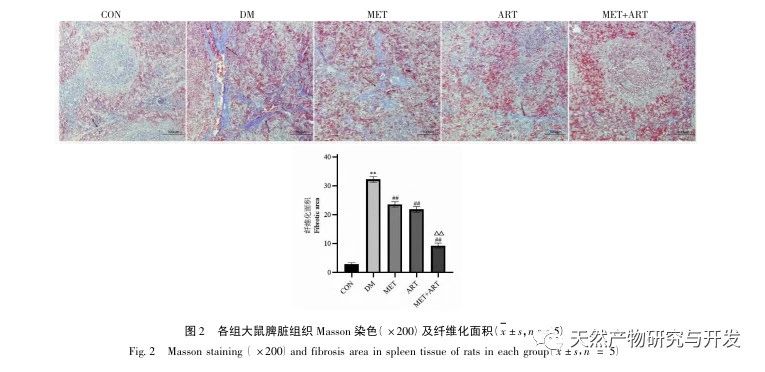
The spleen is the largest immune organ in the human body, and its functions mainly include blood filtration, red blood cells, aging of antigens and foreign bodies, and immune response. T2DM is a group of metabolic diseases, and long-term hyperglycemia can cause oxidative stress and damage to multiple organs. Under oxidative stress conditions, abnormal cytokines are produced in the spleen tissue, leading to spleen enlargement and fibrosis, resulting in spleen damage in patients. When the spleen tissue undergoes fibrosis, the intima of the central artery thickens and the surrounding collagen fibers proliferate, limiting the expansion of the splenic sinusoids and leading to a decrease in blood storage function, resulting in insufficient blood flow and damage to its original physiological functions. The preliminary research of the research group found that T2DM rats can effectively exert drug effects without causing liver toxicity at an ART concentration of 50mg/kg. Therefore, it was determined as the final concentration of the experiment. In this experiment, an SD rat model was established, and metformin, a commonly used drug for treating T2DM, was used as a positive control. HE staining showed that the central artery of the spleen in T2DM rats was thickened and the splenic cord edge was narrow. After medication, the spleen structure improved. Masson staining showed that the collagen fibers around the central artery and vein in the DM group were increased compared to the CON group, while the deposition of blue fibers in each medication group was reduced, and the difference was statistically significant, which to some extent suggests that ART has a protective effect on spleen structure and fibrosis.
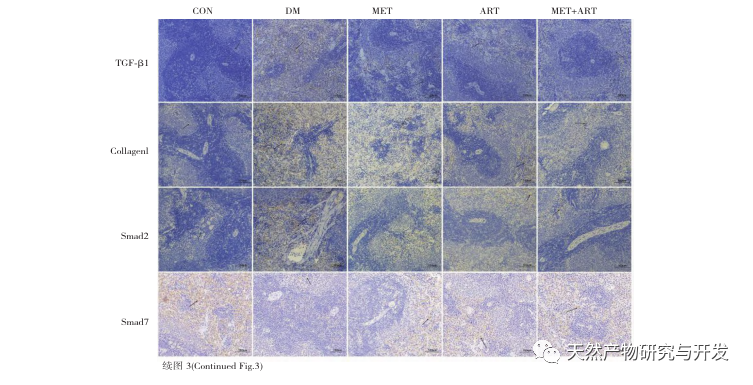
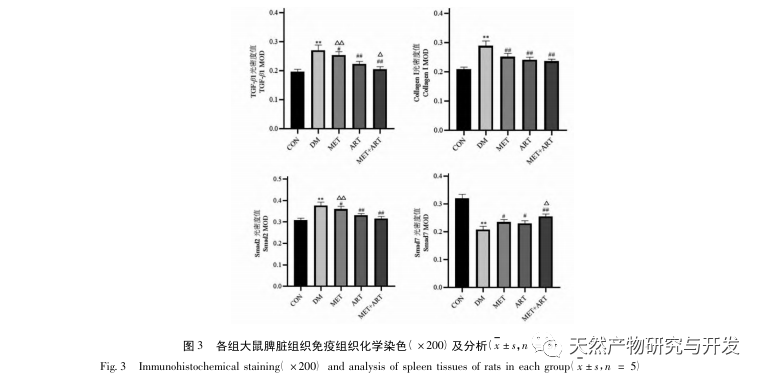
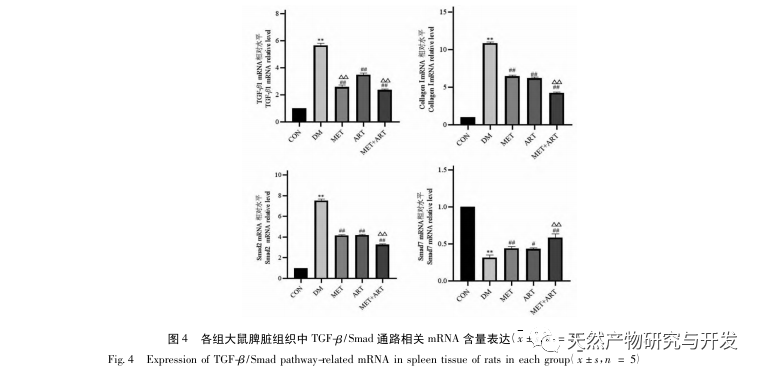
The principle of fibrosis is the pathological process of necrosis of organ parenchymal cells caused by inflammation, abnormal increase and excessive deposition of extracellular matrix (ECM) in tissues, which is also a common symptom of T2DM, including renal fibrosis, pulmonary fibrosis, liver fibrosis, etc. The more fibrous connective tissue in tissues, the easier it is for cells to die, ultimately leading to organ failure. The mechanism of fibrosis is mainly related to the TGF – β/Smad pathway. TGF – β is an important factor in fibrosis, regulating cell growth and apoptosis, including three subtypes. Among them, TGF – β 1 has the strongest activity and plays an important role in the fibrosis process. On the one hand, it promotes the production of ECM and induces fibrosis through its own signaling pathway. On the other hand, it can inhibit the production of matrix metalloproteinases (MMPs) and promote the increase of collagen, exacerbating fibrosis. The recombinant human protein family (smad family member) is a downstream key receptor protein family of TGF – β, including activated types such as Smad2, Smad3, Smad5, and inhibitory types mainly including smad7. Smad7, as a key negative regulator of TGF – β signaling, can inhibit fibrosis by blocking receptor activity, inducing receptor degradation, or interfering with Smad2/3-DNA binding. When tissue fibrosis occurs in patients with diabetes, the expression of TGF – β 1 increases and binds specifically to Smad2 and Smad3. Smad7 is inhibited, which increases the signal transmission from cell membrane to nucleus, thus activating the downstream target gene to promote fibrosis. Research shows that when TGF – β/Smad pathway is activated, the downstream target gene Collagen I will also increase in the deposition of tissue, thus aggravating the degree of tissue fibrosis.
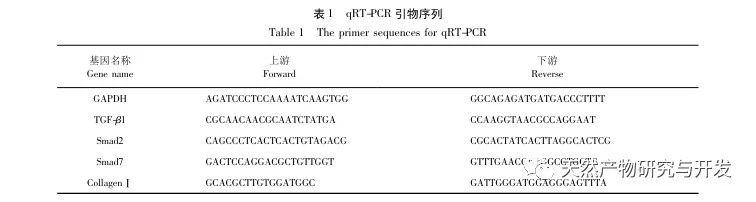
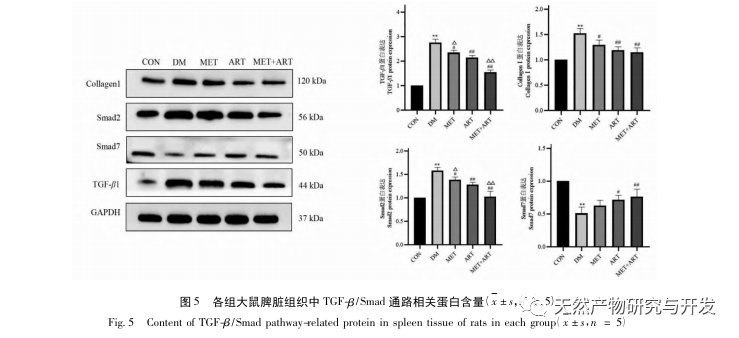
Zhang et al. found that high-dose zinc can prevent and treat splenic fibrosis, and its mechanism may be achieved by reducing the content of TGF – β, Collagen I, and α – smooth muscle actin (α – SMA) in splenic tissue, thereby increasing ECM degradation. Some scholars have also found that TGF – β/Smad signaling pathway is involved in the process of diabetes target organ fibrosis. After treatment, it can improve diabetes target organ fibrosis by reducing the expression of Collagen I, TGF – β, Smad2, Smad3. In this experiment, it was found through immunohistochemistry, Western blot, and qRT PCR that the content of TGF – β 1, Smad2, and Collagen I in the spleen tissue of DM group rats was significantly higher than that of CON group, while the expression of Smad7 was decreased. The protein and mRNA expression levels of TGF – β 1, Smad2, and Collagen I were significantly reduced, and the content of Smad7 was significantly increased in each medication group, with statistical differences consistent with the above results.
To sum up, ART can not only reduce the blood sugar level of T2DM rats, but also have great prospects for the changes of spleen index, spleen weight and spleen structure of T2DM rats. It also reveals that ART has a certain role in the prevention and treatment of spleen fibrosis in T2DM rats, and the effect of the combination group seems to be more significant, and its mechanism may also be related to the inhibition of TGF – β/Smad signaling pathway, which provides a theoretical basis for the study of drug treatment of spleen injury and fibrosis in type 2 diabetes rats.
